
Abtrace welcomes the publication of Fit for the Future: The 10-Year Health Plan for England as a clear articulation of the structural, clinical, and technological reforms needed to place the NHS on a more sustainable and equitable footing. The Plan focuses on three central shifts, from hospital to community, from analogue to digital, and from sickness to prevention. For those who have digested Lord Darzi’s recent report, these principles will come as no surprise; conceptually they are essential for a sustainable public health system, but how will the NHS turn headline grabbing notions into realised operations?
Our response unpacks how these shifts can be made deliverable and durable within the constraints of workforce pressure, financial limitation, and operational complexity: particularly in primary care, where much of the Plan’s success will be determined.
The ambition to move more care closer to home is both clinically sound and financially necessary. Investing in community-based models offers the opportunity to improve access, reduce acute demand, and manage long-term conditions earlier.
However, this transition will only be successful if it is accompanied by:
The proposed creation of Neighbourhood Health Centres and enhanced primary care roles is welcomed. However, without embedded digital infrastructure and smart care coordination, these hubs may simply inherit the fragmentation they are meant to resolve. Without doubt, the extended accessibility that neighbourhood hubs will offer is essential. However, those who have worked at the Primary Care coalface understand how often ‘proactive care’ is delivered opportunistically. Interactions such as ‘I’m sorry to hear your throat is sore, may we check your blood pressure whilst you are here?’ are commonplace, and are enabled through clear signposting of patient requirements. For Neighbourhood Health Centres to ease Primary Care pressure, the system needs to enable shared records and easy identification of opportunities for proactive care.
The Plan outlines a positive trajectory for digital transformation, particularly through a unified NHS App, integrated patient records, and the development of secure messaging and booking systems.
Yet it is essential that this transformation is not overly focused on patient-facing platforms alone, but also on the tools clinicians use every day. Too often, digital solutions have added administrative load rather than reducing it. To avoid repeating this pattern, technology must be:
Crucially, practices need IT systems that support not just record-keeping, but active, intelligent care management.
It’s exciting to see prevention placed at the heart of the Plan; from obesity and smoking cessation to cardiovascular and mental health risk, there’s huge untapped potential. Momentum is building for the long-term shift towards prevention – something that we have been advocating for to unlock sustainable population health management.
However, whilst national policy can provide population-level levers, preventive care still happens patient by patient, often in the consultation room, or through structured monitoring and follow-up.
This shift requires:
Without operationalising prevention in day-to-day general practice, national targets will remain aspirational.
Abtrace’s mission is closely aligned with the priorities set out in this 10-Year Plan. We believe that to shift care earlier, closer, and smarter, clinicians must be supported with intelligent tools that work with them, not around them.
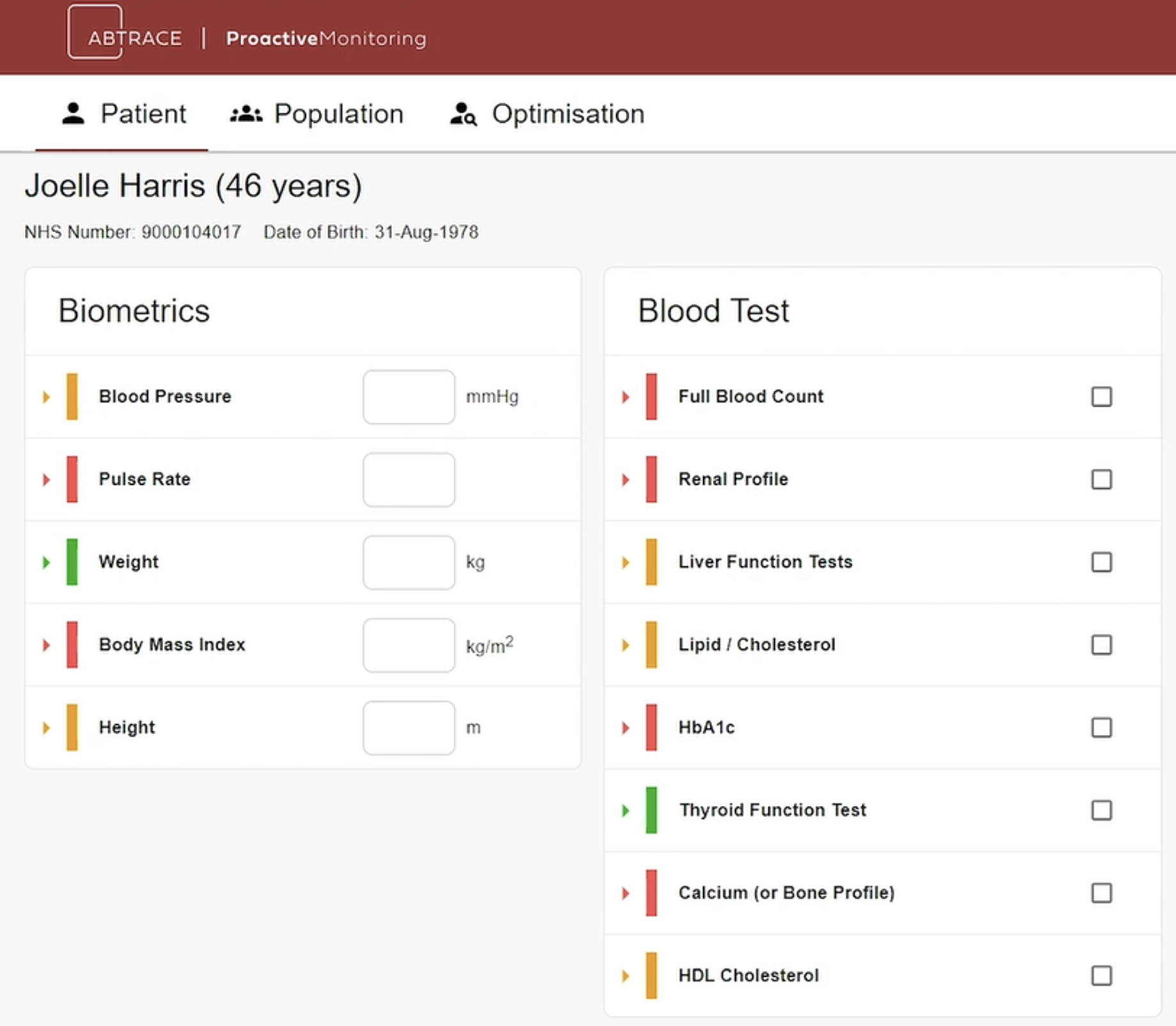
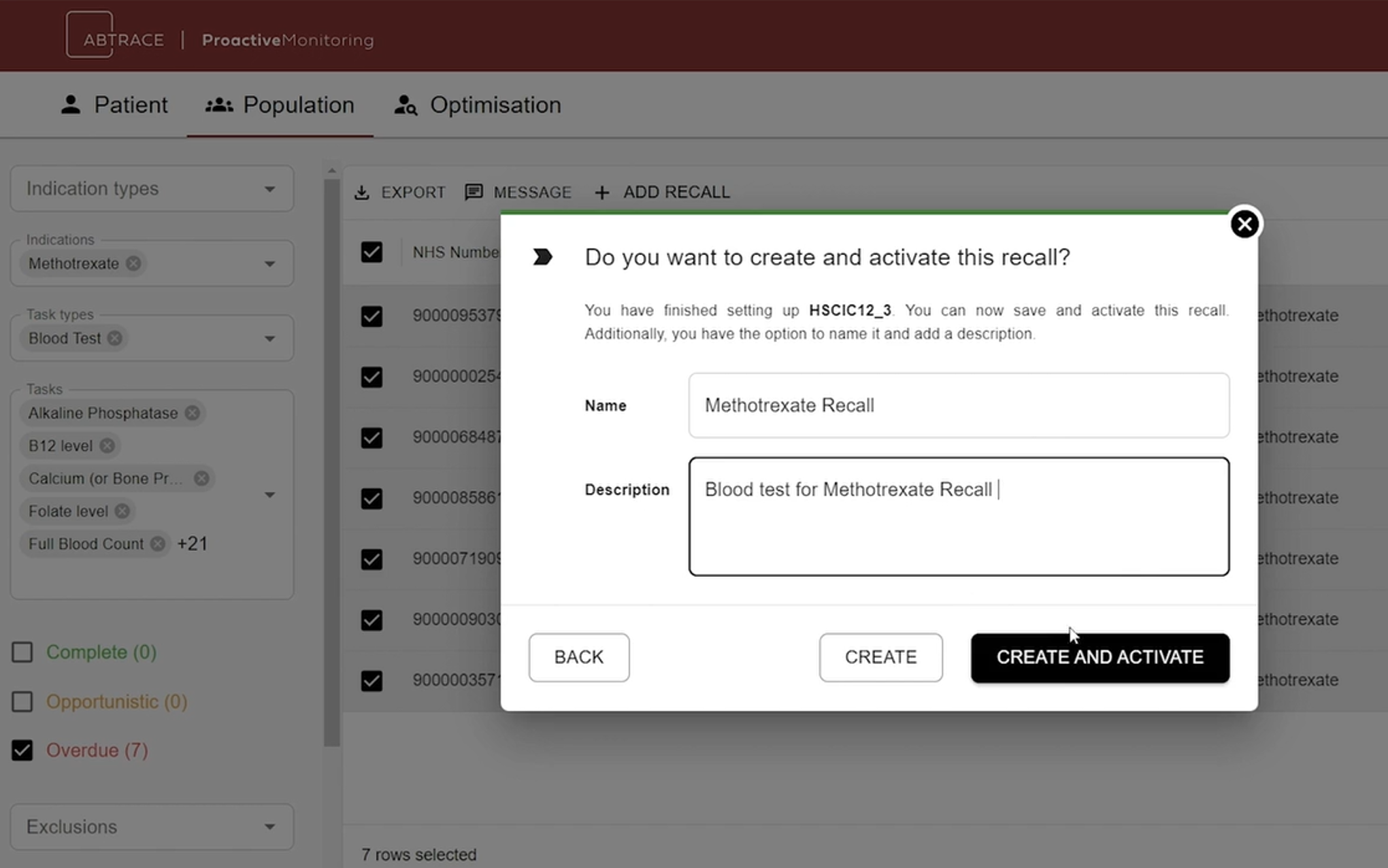
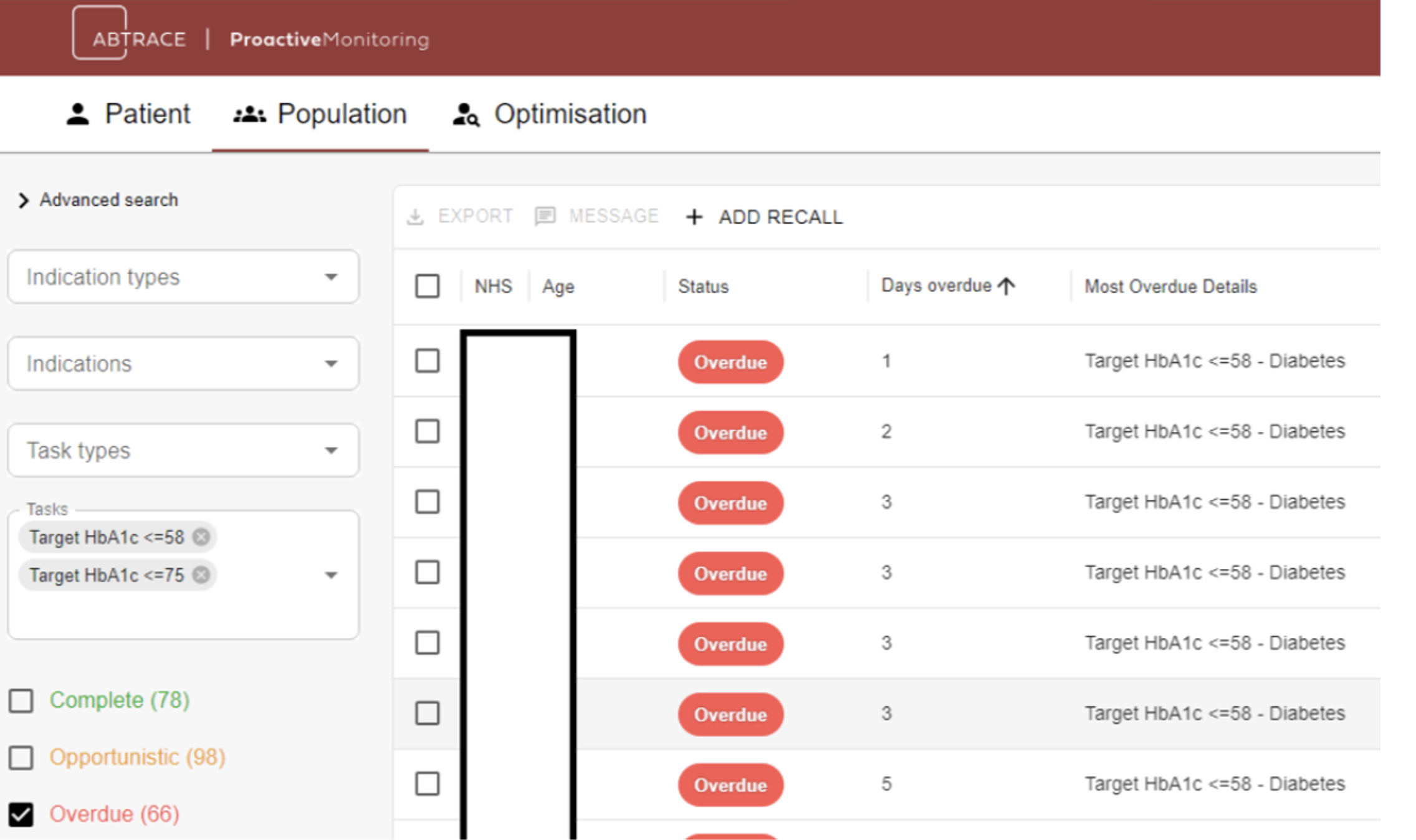
Our software platform is already being used in NHS primary care to:
These tools are designed to operate within existing systems (EMIS, SystmOne) and workflows, making digital transformation not just possible, but practical.
As the NHS looks to implement the Plan’s ambitions at pace, we believe that targeted support for embedded, safety-focused technologies, particularly those that enable primary care teams to do more with less, will be key to success.
Abtrace is committed to working with NHS partners across ICBs, PCNs, and practices to realise the shared vision of a preventive, digitally enabled, community-centred health service.
Dr. Simon Doyle, Senior Digital Health GP
Abtrace, July 2025